Does marijuana cause schizophrenia?
Erik Messamore, MD, PhD
Introduction
The risk of schizophrenia jumps by more than 300% among regular cannabis users. This is a well-established fact.
What has been unclear is whether this additional risk is actually caused by the cannabis exposure, or whether the association is secondary to some other process (for example, maybe people destined to develop schizophrenia happen to find cannabis more useful than the average person and therefore use it more often).
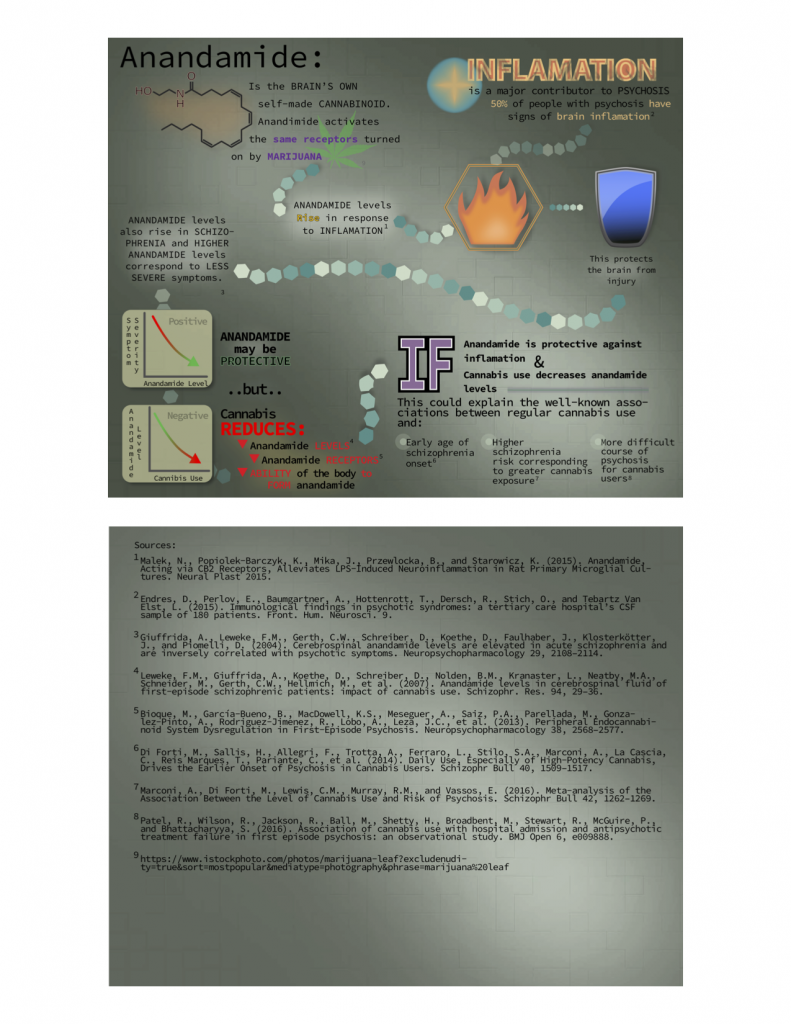
Emerging scientific findings are more supportive of a causal relationship – that regular cannabis use actually drives the extra schizophrenia risk. The anandamide-depletion hypothesis can explain how regular cannabis makes schizophrenia more likely.
The hypothesis is based on findings that:
- Inflammation is a major contributor to psychosis
- The brain’s own cannabinoid substance, anandamide, rises during inflammation and is part of a natural anti-inflammatory response
- Regular exposure to plant-derived cannabinoids reduces the brain’s ability to produce its own cannabinoids
This would make the frequent marijuana user more vulnerable to the effects of brain inflammation and thus more prone to develop a schizophrenia-like psychosis.
Regular cannabis use is a schizophrenia risk factor
Frequent users of cannabis are diagnosed with schizophrenia much more often than non-users. Schizophrenia begins at earlier ages in cannabis users, and higher exposure to cannabis in early life corresponds to greater risk of schizophrenia later in life. Genetic analyses using a specialized approach called Mendelian Randomization suggest that the association is causative, not coincidental.
Anandamide, the brain’s own cannabinoid, may protect against inflammation and psychosis
Anandamide levels rise in response to inflammation in the central nervous system. The anandamide response appears designed to reduce inflammation, and inflammation is an important pathway to persistent psychosis. A recent study showed evidence of brain inflammation in half of consecutively-screened individuals with psychosis. The brain’s anti-inflammatory anandamide response may limit the progression from inflammation to psychosis.
Anandamide defense system, low in schizophrenia, is further lowered by regular cannabis use
People with schizophrenia appear to have a diminished anandamide response. Anandamide receptor levels appear lower in schizophrenia. Anandamide-forming enzymes are also reduced in schizophrenia. Both types of change (diminished receptors and reduced enzymes of formation) are accentuated by regular cannabis use. Cannabis use also corresponds to higher levels of anandamide-destroying enzymes. These findings may explain why anandamide levels in the CNS are lower in people who regularly use cannabis.
A possible explanation for the cannabis-schizophrenia connection
It appears that prolonged exposure to exogenous plant-derived cannabinoids reduces the body’s ability to form its major endogenous cannabinoid, anandamide. Diminished anandamide response renders the brain more susceptible to inflammatory insults. This hypothesis could also account for findings of cannabis-associated schizophrenia-like psychosis being less likely to respond to first-line antipsychotic medication. Under this hypothesis, cannabis-associated psychosis may have more to do with exaggerated inflammation than with exaggerated dopamine signals. These observations are based on a relatively small number of studies, but existing data suggest a mechanism to explain widely-replicated observations of higher schizophrenia risk in regular cannabis users.